That's what David Maahs, MD, PhD, a Stanford Medicine professor of paediatrics, and his colleagues found when they moderated a series of 16 focus groups -- eight each in rural northern California and Florida -- to illuminate barriers to diabetes care and technology use among underserved communities in the United States.
Eighty-six adult participants agreed to be interviewed in hour-long Zoom sessions. Many were recruited through Federally Qualified Health Centres; others were patients recently hospitalized for diabetic ketoacidosis, and some had high blood sugar -- levels of haemoglobin A1c, a glucose marker, above 9% -- but had skipped two or more endocrinologist visits in a row.
Maahs and his colleagues from the University of Florida have been piloting a project called ECHO Diabetes, based on the Extension for Community Health Outcomes model developed at the University of New Mexico for hepatitis C.
The goal of the project, Maahs said, is "to raise, through tele-education, the level of care primary doctors can provide in their own communities." As part of this effort, the Stanford and Florida teams wanted to hear directly from underserved type 1 diabetes patients, which is why they conducted focus groups, recording and transcribing the interviews.
Often, when asked about challenges they encountered in trying to manage their disease, participants made revealing comments. One, for example, was repeatedly denied a continuous glucose monitoring device, and reported being "in a diabetic coma three times this year because they won't give me what I need to maintain" healthy blood sugar levels.
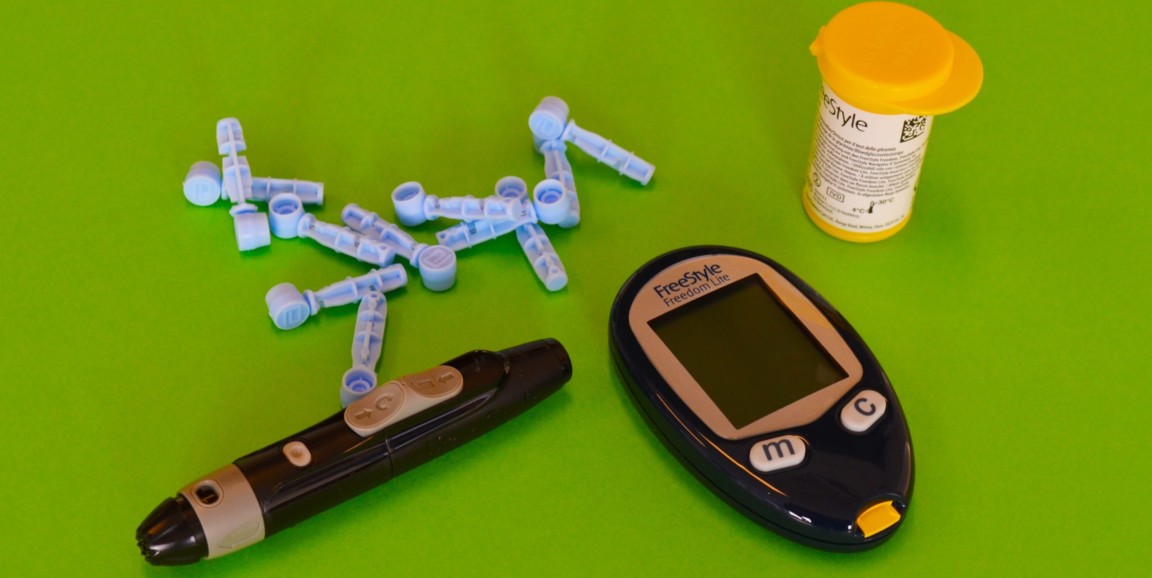
Photo by Diabetesmagazijn.nl
Another was prescribed insulin shots, but not informed about how to move to advanced care, such as an insulin pump. Instead, the patient said, her clinician "complained the whole time, telling me, 'You're going to die, your kids are going to not have a mama.'"
To Maahs, who is division chief of paediatric endocrinology, these kinds of responses were upsetting, but not surprising. "It's always so powerful to hear patients' voices on how such barriers have affected their lives," he said. "Many had never been asked about their experiences before, and, well, they sure told us."
Maahs' research was published in July in Diabetes Care. Ashby Walker, PhD, from the University of Florida Diabetes Institute, is the first author.
Improving bedside manner, educating more providers
Of the barriers that patients identified, unsympathetic endocrinologists topped the list. One participant said, "I prep myself to go in for what feels like an attack when I am looking for help and support." Another heard, "You're using way too many blood glucose strips." But later, when the same patient asked for a continuous glucose monitor, the doctor asked, "Well, are you too lazy to test your blood sugars?"
The researchers also found that, at the time they were interviewed, more than 50% of participants hadn't seen an endocrinologist in a year, never mind following through on the recommended four check-ups annually.
"It's unfortunate, and a reminder to physicians that how they speak with patients is really important," Maahs remarked. "We're doing a lot of research on ways to reduce implicit biases at the provider level."
Meanwhile, he and his colleagues have expanded the project, launching a clinical trial focused on training primary care physicians who may lack expertise in general diabetes management. Often, they are the main or only health care providers in underserved areas, Maahs said. The team is testing whether weekly tele-education sessions "leads to improvements in both provider job satisfaction and patient health," he said.
Diabetes management is two-tiered, he said. "Some patients, based on insurance status and where they live, receive cutting-edge care; others who lack insurance or live in rural areas receive outdated or minimal care."
"With our program, we aim to equip more providers with the relevant knowledge so patients in disadvantaged communities receive better care than what they currently have," he said.
https://scopeblog.stanford.edu/2021/07/26/managing-type-1-diabetes-voices-of-the-underserved/
No comments:
Post a Comment