Rural areas in India are also experiencing
Keep reading to learn more about diabetes in India, including prevalence, some reasons it is so common, and more.

In India, more than
Overall, females have a higher risk of developing diabetes than males, but as both groups get older, this risk decreases.
Although diabetes figures are high, researchers estimate that 57% of cases remain undiagnosed. This is particularly concerning, as the risk of serious complications increases when people do not take medication to control their blood sugar.
There are several theories that attempt to explain why diabetes cases are rapidly increasing in India. The sections below look at some of these in more detail.
Physiological differences
People of South Asian ancestry tend to have a
Because typical Western diets and fast foods are growing in popularity, especially in urban environments, so is fat and sugar consumption.
When the body cannot efficiently clear glucose, this increases metabolic load and insulin resistance and puts a person at risk of developing diabetes.
Perception of diabetes
People tend to view diabetes as a “new” condition in rural areas, and general awareness of the condition is low.
In a small
Because people typically view doctors as the best sources of diabetes information, and because they may not have access to other resources, these short consultations have a significant effect on the number of complications that people experience.
Changes in farming practices
Government shops, or fair price shops, are a type of public distribution system that offers rural communities low cost food to improve people’s nutritional health. These foods include white rice, wheat, sugar, and pulses.
However,
In place of traditional foods, people are now consuming more polished white rice and refined sugar, the consumption of which causes spikes in blood glucose levels.
Sweet cuisines
The consumption of sugary sweets is a staple of Indian culture and an integral part of ancient traditions and religious festivals.
According to one
In cities, sugary drinks and sweetened foods are cheap and readily available, which is increasing people’s risk of developing obesity and type 2 diabetes.
Social stress
Many people report that stress or tension was the cause of their diabetes.
A
As Indian doctors talk more about social stress as a risk factor for diabetes than those in the United States, these beliefs likely originate from information that people receive at healthcare consultations.
Because lower income groups typically have less access to healthcare, this could explain why they do not think that social stress causes diabetes.
Increased availability of processed foods
Like big cities, rural villages are now selling cheaper processed foods. Due to recent changes in imports and economic policies, the variety and availability of processed foods have expanded, and people’s preferences are shifting toward fatty sugary snacks and meals. This trend is
- regularly urinating at night
- feeling thirsty all the time
- losing weight without trying
- feeling hungry all the time
- feeling tired all the time
- having sores that take a while to heal
- experiencing more infections than usual
Treatment varies depending on the type of diabetes a person has. The following sections look at some treatment options for both type 1 and type 2 diabetes.
Type 1 diabetes
When a person has type 1 diabetes, their pancreas stops producing insulin. To treat this condition, a doctor prescribes an artificial form of insulin that a person takes several times per day and with meals.
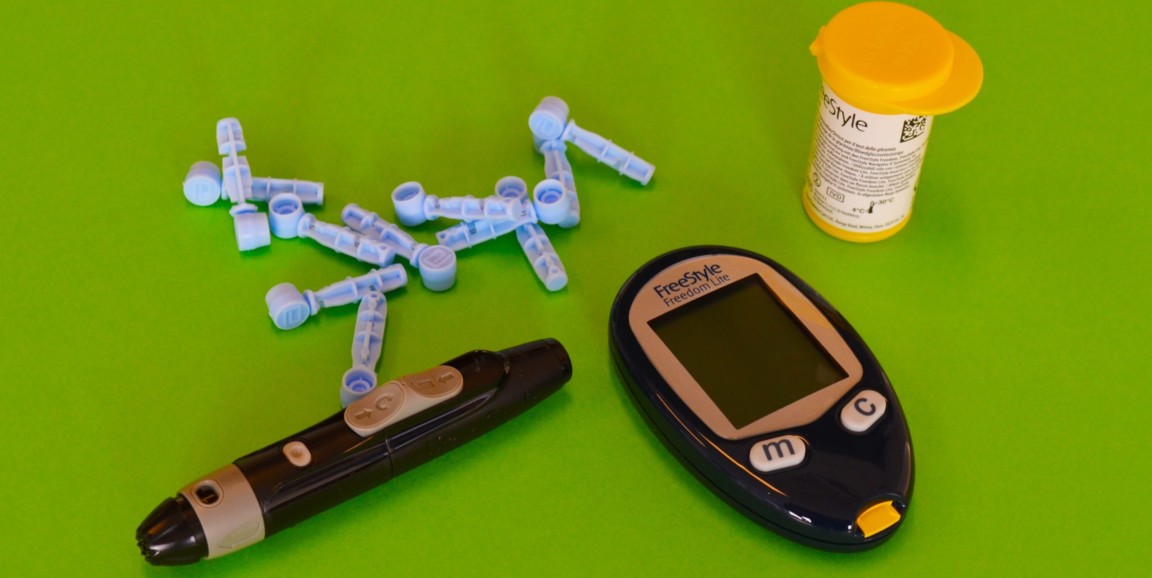
People take insulin using a needle and syringe, or an insulin pen. If someone needs a steady supply of insulin throughout the day, they may prefer using an insulin pump.
Insulin does not come in tablet form because stomach acid destroys it.
Type 2 diabetes
Many people with type 2 diabetes need to take medication and insulin to control their symptoms. Some treatments come in tablet form, and a person may take a combination of different medications to keep their blood sugar levels stable.
Diabetes is an escalating health problem in India. One recent review suggests that the lifetime risk of males developing diabetes from the age of 20 years is
Diabetes cases are increasing because the country is undergoing a period of urbanization, meaning that more people are moving to bigger cities for employment. Urbanized areas and cities promote lifestyle habits that are more sedentary, which is a risk factor for both obesity and diabetes.
The bodies of people of South Asian ancestry respond differently to sugary and fatty foods than the bodies of people of European ancestry, and because processed Western foods are growing in popularity in India, so is the risk of diabetes.



![Professor of Physics Paul Dastoor holds up a non-invasive, printable saliva test strip for diabetics at the University of Newcastle, New South Wales, Australia [Courtesy of University of Newcastle via Reuters]](https://www.aljazeera.com/wp-content/uploads/2021/07/2021-07-13T010507Z_1903186655_RC2TJ59UYJ3P_RTRMADP_3_HEALTH-AUSTRALIA-DIABETES.jpg?resize=770%2C513)

